INDICATION:
Juxtapid is a microsomal triglyceride transfer protein inhibitor indicated as an adjunct to a low-fat diet and other lipid-lowering treatments, including LDL apheresis where available, to reduce low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), apolipoprotein B (apo B), and non-high-density lipoprotein cholesterol (non-HDL-C) in patients with homozygous familial hypercholesterolemia (HoFH).
LIMITATIONS OF USE:
The safety and effectiveness of Juxtapid have not been established in patients with hypercholesterolemia who do not have HoFH, including those with heterozygous familial hypercholesterolemia (HeFH). The effect of Juxtapid on cardiovascular morbidity and mortality has not been determined.
WARNING: RISK OF HEPATOTOXICITY
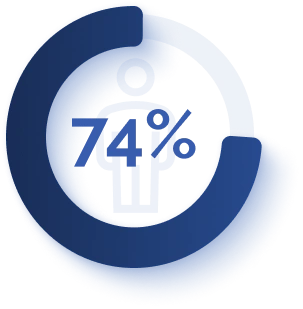
Juxtapid can cause elevations in transaminases. In the Juxtapid clinical trial, 10 (34%) of the 29 patients treated with Juxtapid had at least one elevation in alanine aminotransferase (ALT) or aspartate aminotransferase (AST) ≥3x upper limit of normal (ULN). There were no concomitant clinically meaningful elevations of total bilirubin, international normalized ratio (INR), or alkaline phosphatase.
Juxtapid also increases hepatic fat, with or without concomitant increases in transaminases. The median absolute increase in hepatic fat was 6% after both 26 and 78 weeks of treatment, from 1% at baseline, measured by magnetic resonance spectroscopy. Hepatic steatosis associated with Juxtapid treatment may be a risk factor for progressive liver disease, including steatohepatitis and cirrhosis.
Measure ALT, AST, alkaline phosphatase, and total bilirubin before initiating treatment and then ALT and AST regularly as recommended. During treatment, adjust the dose of Juxtapid if the ALT or AST are ≥3x ULN. Discontinue Juxtapid for clinically significant liver toxicity.
Because of the risk of hepatotoxicity, Juxtapid is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Juxtapid REMS Program.
Prescribe Juxtapid only to patients with a clinical or laboratory diagnosis consistent with HoFH. The safety and effectiveness of Juxtapid have not been established in patients with hypercholesterolemia who do not have HoFH.
CONTRAINDICATIONS:
- Pregnancy
- Concomitant administration of moderate or strong CYP3A4 inhibitors
- Moderate or severe hepatic impairment or active liver disease including unexplained persistent elevations of serum transaminases
WARNINGS AND PRECAUTIONS
Juxtapid can cause elevations in transaminases and hepatic steatosis. Although cases of hepatic failure have not been reported, there is concern that Juxtapid could induce steatohepatitis, which can progress to cirrhosis over several years. Modify the dose of Juxtapid if elevations of transaminases are observed and discontinue Juxtapid for persistent or clinically significant elevations. If transaminase elevations are accompanied by clinical symptoms of liver injury, such as nausea, vomiting, abdominal pain, fever, jaundice, lethargy, flu-like-symptoms, increases in bilirubin ≥2x ULN, or active liver disease, discontinue treatment with Juxtapid and identify the probable cause. Use Juxtapid with caution when co-administered with agents known to be hepatotoxic. Alcohol may increase levels of hepatic fat and induce or exacerbate liver injury.
Measure ALT, AST, alkaline phosphatase, and total bilirubin before initiating treatment. During the first year, measure liver-related tests (ALT and AST, at a minimum) prior to each increase in dose or monthly, whichever occurs first. After the first year, do these tests at least every 3 months and before any increase in dose.
Juxtapid may cause fetal harm when administered to a pregnant woman. Females of reproductive potential should have a negative pregnancy test before starting Juxtapid and should use effective contraception during therapy with Juxtapid. The recommended maximum dosage of Juxtapid is 40 mg daily when used concomitantly with oral contraceptives.
Given its mechanism of action in the small intestine, Juxtapid may reduce the absorption of fat-soluble nutrients. Patients treated with Juxtapid should take daily supplements that contain 400 international units vitamin E and at least 200 mg linoleic acid, 210 mg alpha-linolenic acid (ALA), 110 mg eicosapentaenoic acid (EPA), and 80 mg docosahexaenoic acid (DHA).
Gastrointestinal adverse reactions are common and may lead to treatment discontinuation. Instruct patients to stop Juxtapid and contact their healthcare provider if severe diarrhea occurs, or if they experience symptoms of volume depletion such as lightheadedness, decreased urine output, or tiredness. In such cases, consider reducing the dose or suspending use of Juxtapid. To reduce the risk of gastrointestinal adverse reactions, patients should adhere to a low-fat diet supplying less than 20% of energy from fat and the dosage of Juxtapid should be increased gradually.
Weak CYP3A4 inhibitors can increase the exposure of lomitapide approximately 2-fold; therefore, when Juxtapid is administered with weak CYP3A4 inhibitors, the dose of Juxtapid should be decreased by half and the recommended maximum dosage of Juxtapid is 30 mg daily. The recommended maximum dosage is 40 mg daily when used concomitantly with oral contraceptives. Strong and moderate CYP3A4 inhibitors should not be used with Juxtapid. Patients taking Juxtapid 5 mg daily may continue with the same dosage.
Due to risk of myopathy associated with simvastatin or lovastatin, doses of these agents should be limited when co-administered with Juxtapid.
Juxtapid increases the plasma concentrations of warfarin. Increases or decreases in the dose of Juxtapid may lead to supra- or subtherapeutic anticoagulation, respectively. Patients taking warfarin should undergo regular monitoring of the INR, especially after any changes in Juxtapid dosage.
Avoid use of Juxtapid in patients with rare hereditary diseases of galactose intolerance.
ADVERSE REACTIONS:
The most common adverse reactions were gastrointestinal, reported by 27 (93%) of 29 patients. Adverse reactions reported by 8 (28%) or more patients in the HoFH clinical trial included diarrhea, nausea, vomiting, dyspepsia and abdominal pain. Other common adverse reactions, reported by 5 to 7 (17-24%) patients, included weight loss, abdominal discomfort, abdominal distension, constipation, flatulence, increased ALT, chest pain, influenza, nasopharyngitis, and fatigue.
REPORTING OF ADVERSE REACTIONS:
All healthcare professionals should report all suspected adverse reactions. Please contact Chiesi Farmaceutici S.p.A. at 1-888-661-9260 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Please see Full Prescribing Information including BOXED WARNING for the risk of hepatotoxicity.